Webinar: Translational Medicine Approach to COVID-19 in Saudi Arabia
Our panelists discuss translational medicine in Saudi Arabia. This discussion focused specifically on the approach that translational medicine has had to COVID-19. Our panelists are drawn from Ibn Khaldun Fellows and our sponsor, KACST. Among them they bring a broad perspective on the current translational medicine partnerships in Saudi Arabia and a vision of where to go from here.
Date: Wednesday, September 16, 2020, 9:00-10:30 PM KSA (2 PM Boston)
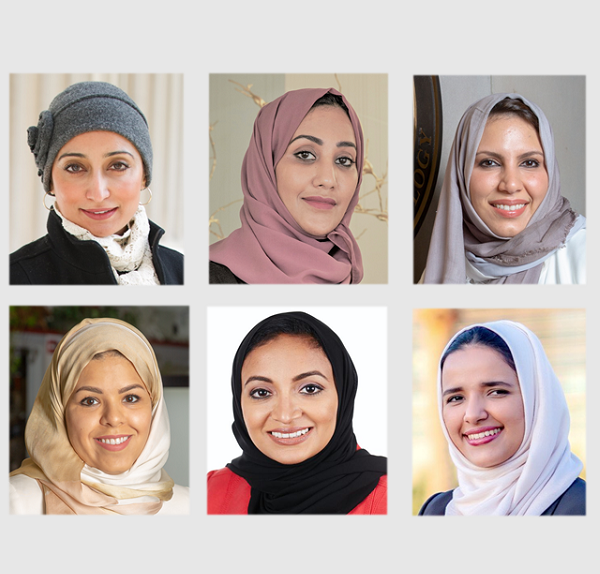
Panelists:
Dr. Sanaa Al Attas, Associate Professor, King Abdulaziz University
Dr. Mariam AlEissa, Head of Molecular Genetics Department, Saudi Centers for Disease Prevention and Control
Dr. Sufana AlMashhadi, Director, Innovation Center, King Fahad Medical City
Dr. Shada AlSalamah, Assistant Professor, King Saud University
Dr. Malak Althagafi, Deputy General Director, Research and Innovation, KACST
Moderator: Dr. Seba Nadeef, IBK Fellow, KAUST PhD
Webinar Transcript
DR. SEBA NADEEF: --narrating today, this session, and I'm very glad to be here. Let me start first by introducing Dr. Kamal Youcef-Toumi. Dr. Kamal is a faculty member in the Mechanical Engineering Department at MIT where he is the director of the Mechatronics Research Lab. He is also the co-director of the Center for Complex System at MIT and KACST, and he is also the director of the KACST MIT Ibn Khaldun Fellowship for Saudi Women, the organizers of today's event.
Good evening, Dr. Kamal, and we are all great to have you here today. So if you can please tell us more about the fellowship and the seminars that you and the team are organizing.
KAMAL YOUCEF-TOUMI: [ARABIC]. Hello, everyone, and welcome to today's webinar. Shukran Dr Seba. Yes, I also would like to thank the panelists for making the time to prepare and also be part of this important webinar. Also our team from the MIT side-- Theresa, and Dorothy, and Nadiyah for putting a lot of these programs together. So these webinar series are meant to inform the public at large.
And at the same time, to highlight all the contributions from our fellows. These are all of the Saudi women that were handpicked, both by KACST and MIT. And a lot of them have spent time at MIT at least a year, some of them a year and a half, and then others, I think two years, working in many different fields. So this is maybe a brief summary of the objectives of these webinar series. And then we will have different topics you know as we go forward.
And maybe a brief comment on the program for those participants who are not familiar with the Ibn Khaldun fellowship program. So it was established through the MIT KFUPM with King Fahd University of Petroleum and Minerals collaboration. This was almost 12 years ago. And Saudi Aramco expanded the program in 2013, and then in March of 2018 we moved it to KACST, and now it's been with the sponsorship and collaboration with KACST.
And the last word is I want to let everyone know about the capability of our fellows -- very, very distinguished women. All of their contributions that they have done at MIT-- both in the technical and non-technical aspects. And more importantly, the great work that they are doing back in the kingdom. So we plan to continue. to work with the previous fellows and also with the current ones. And all of this for the benefit not only of the kingdom but for mankind. Thank you, and sorry for taking too much of your time, Dr. Seba.
DR. SEBA NADEEF: Thank you very much, Dr. Kamal, for your support always for the science and the ladies in science always. And we are happy today here to have Dr. Sufana Almashhadi, Director of Innovation Center at King Fahd Medical City. Dr. Shada Alsalamah, professor at King's College University and Dr. Mariam AlEissa, Head of Molecular Genetics Departments, Saudi Center's for Disease Prevention and Control. Dr. Sana Al Attas, Associate Professor at King Abdulaziz University, and Dr. Malak Althagafi, physician scientist in clinical pathology and Deputy General Director of Research and Innovation at KACST.
Welcome, our guests. It's our pleasure to welcome you all here today. As Dr. Kamal mentioned, our speakers are coming from different backgrounds, and they are affiliated to different top research institutes and universities in the kingdom, but they share a common interest which is their passion about science and driving change and innovation in Saudi Arabia. Thank you very much for being here, and it will be great if each one of you could introduce herself to the audience with your background, and your interests, and your current work. Let me start first with Dr. Sufana.
DR. SUFANA ALMASHHADI: Thank you, Seba. Salamu alaykum. Good evening, everyone. Or good afternoon, wherever you are in the world. Thank you so much for having us. Thank you, Professor Kamal, for your great support and the MIT Ibn Khaldun fellowship management team and the KACST for supporting this amazing program. So I'm really passionate about science and specifically about translating our information and our understanding of the human brain. And specifically, my background-- so I gained my PhD in neurodegenerative disorders.
Which means, how do we understand more? What does the aging process? And how can you preserve your cognitive functions for even healthier, better life? So there are many aspects of the brain that really fascinate me. Recently I have been involved in transforming or translating the research work into more sustained kinds of impactful projects that can have a return of investment or can even transform from the bench to having a project that is tangible and that is accessible by the community and by the society.
So I'm very much interested in this area specifically. However, I'm still practicing as a neuroscientist at King Fahd Medical City, and I'm maintaining my research affiliate with MIT.
DR. SEBA NADEEF: Thank you very much, Dr. Sufana. What about you, Dr. Shada?
DR. SHADA ALSALAMAH: [ARABIC]. Thank you very much, Dr. Seba. It's a pleasure to be here, and I thank you for organizing-- MIT, Ibn Khaldun fellowship for organizing this. Thank you, Dr. Kamal, Dorothy, and the rest of the team. So in a nutshell, I am an academic, a mentor, a public speaker, an author, and entrepreneur, a former Ibn Khaldun MIT fellow, and also a patient centricity advocate.
Now, currently I am an Assistant Professor of Health Care Information Systems Security at King Saud University in Riyadh. I'm also a consultant at the Department of Digital Health and Innovation at the World Health Organization in Geneva. And since the beginning of the pandemic, I've been helping and consulting for the National Health Command Center and the Ministry of Health and Riyadh in order to support with their COVID-19 response.
I also serve on a number of national and international boards in relation to emerging technologies like Blockchain, Artificial Intelligence and Information Security, including the Organization for Economic Co-operation and Development blockchain expert policy advisory board in Paris, the International Association for Trusted Blockchain Applications in Brussels in Belgium, also the Dev Master AI training company in Los Angeles, California, and finally, the Saudi Association for Information Security in Riyadh, Saudi Arabia. Over to you, Seba. Thank you very much.
DR. SEBA NADEEF: Thank you very much, Dr. Shada. What about you Dr. Mariam?
DR. MARIAM ALEISSA: Hi, I'm Mariam AlEissa. I used to be a fellow at MIT, at McGovern Institute of Brain Research, and I'm also affiliated with the Broad Institute of MIT and Harvard. Currently I'm working in the Saudi CDC, and I was fortunate during my time in MIT to award a number of certificates in innovation, entrepreneurship, and leadership. This implicates on my current work where I'm trying to establish the molecular genetics department in my job.
DR. SEBA NADEEF: That's great. What about you, Dr. Sana? No Dr. Sana?
DR. SANA AL ATTAS: OK, thank you very much for this kind introduction, Dr. Seba and, of course, first of all, I would like to welcome your, Professor Kamal and all of the panelists from the Ibn Khaldun community and fellowship-- Dorothy, Theresa, the rest, of course. I would like to start another way. I will start by explaining the meaning of translational medicines, and some of my students are with us and have been asking me several times about the exact definition of the translational medicine.
So it's an interdisciplinary branch of the biomedical field as defined by the European Society for Translational Medicine. It's supported by three main pillars which is the bench side, bedside, and community, and the goal of it is to combine disciplines, resources, expertise, and techniques within these three pillars. And preventive, prevention, diagnosis, and therapies. Accordingly, translational medicine is a highly interdisciplinary field. However, the primary goal of which is to improve the global health care system.
As a researcher with a background in virology, having my post doctoral fellowship training at MIT, it has strengthened my research capability in public health. I have carried out research activities that involve multi-disciplinary experts which, in turn, is a form of translational science in a naturally occurring diseases and applying the findings of law or from basic science research to enhance health and well-being in humans.
For example, I was principal and in some other researches, I was a co-investigator to a number of researchers that afforded me a unique interaction with the concentration of the infectious disease and public health experts with an array of expertise in different disciplines. I hope that the interaction between those colleagues will afford me to play a vital role in the development of prevention and control of the current COVID-19 pandemic.
Last November 2019, one of our articles was nominated to win the Sheikh Zayed award for Alternative Prophetic Medicine in Abu Dhabi for research conducted in German laboratories on the use of the active substance, [INAUDIBLE], extracted from camels as an antiviral drug on human cells. Also other recently published papers [INAUDIBLE] find any relationship between some substantial vaccines and the likelihood of COVID-19 infection all over the world.
DR. SEBA NADEEF: Thank you very much, Dr. Sana. And finally, Dr. Malak, what about you?
DR. MALAK ALTHAGAFI: Hi everyone, [ARABIC]. Good evening. I would like to thank the MIT Ibn Khaldun fellowship for having me today as a panelist. I'm a little bit different than all the others. I'm actually not an IBK fellow, but I'm a fellow, their natural competitor across the Charles River, I'm actually a Harvard alumni.
[CHUCKLING]
What is my background in education? I graduated medical school at King Abdulaziz University. I did my postgraduate medical education at Georgetown, UCSF, Harvard, Brigham and Women, Boston Children. I also did my MBA in Medical Management at Johns Hopkins.
Now what I do, I can define myself as a management executive, a physician scientist, as a management executive, currently actually, thanks to KACST and their support to women. So now I'm actually the Director General of the General Directorate for Research Development and Innovation Coordination. I was, as you introduced me, a deputy director just last month for Research, Innovation, and Support.
So that's what I do in KACST. And I'm also a member of many committees, national international committees. What I do as a physician-- I'm actually the director of Satellite Research Administration at King Fahd Medical City where I oversee three departments-- the Department of Genomex, I'm actually the founding chair of it. I'm the Director of the Saudi Human Genome Satellite side there. Also, I oversee the National Neuroscience Research Department and Research Collaboration Department.
As a physician, I'm a consultant subspecialty in molecular genetics, neurophatology, surgical, oncology pathology. So this is me in a nutshell. And I'm an advocate of women in the science, and I'm very glad to be here today to join you as a panelist.
DR. SEBA NADEEF: Thank you all, ladies, for the nice introduction. It's very impressive, and I'm very happy to hear that me, as a scientist, you, as a woman, and also as brave scientists. So before we start, I would like to mention to the audience that if you would like to ask questions before we start, you have the feature Q&A where you can post your question, and it will be answered at the end of the seminar.
So people are asking maybe, what is translational research? In addition to what Dr. Sana said, translational research is the process of applying knowledge from basic biology and clinical trials to techniques and tools that address a critical medical need to improve the health outcome. And nowadays the science and innovation landscape in the Kingdom of Saudi Arabia is currently undergoing massive restructuring of its research, development, and innovation ecosystem.
This change is impressive and rapid for the last five years, and it's part of the vision 2030. So since all of you are coming from different scientific backgrounds, could you please tell us how your background or your scientific contribution can be more related to the translational research in the healthcare field. Let's start with Dr. Shad. Sorry, Dr. Shada.
[CHUCKLING]
DR. SHADA ALSALAMAH: Yes, thank you. Generally speaking, I've been a contributor to the Healthcare Sector Modernization movement and policy-making at the national and international levels. That's for better disease detection, prevention, and also treatment. Now specifically using emerging technologies. Therefore, I have founded and co-founded a number of initiatives that mainly aim to solve local health problems in Saudi Arabia with the potential of a global impact.
And that is at the heart of my research agenda. That's why I collaborate with different subject matter experts and decision and policymakers in Saudi Arabia-- from the Ministry of Health, the Red Cross in Authority, secondary and tertiary hospitals, pharma, dental clinics, also research centers, and universities. This is to mainly create trusted ecosystems where we all, as a team and with my students, we build solutions that can address burning and pressing problems that keep those people or those experts up at night and also to help them make informed decisions.
In the ecosystem and the team collaboration, we develop solutions with a mixture of emerging technologies, including blockchain, artificial intelligence, wearables, mobile technology, and many others in order to enhance the experience of patients and all those other stakeholders involved in the healthcare ecosystem. Thank you, over to you, Seba.
DR. SEBA NADEEF: Thank you, Dr. Shada. What about you, Dr. Sufana?
DR. SUFANA ALMASHHADI: Yes, so I have been recently assigned as the Director of the Innovation Center of King Fahd Medical City which is considered as one of the main biggest tertiary healthcare hospitals in the kingdom. And as we are looking into transforming our healthcare system into a more human-centric approach, I have dedicated my skills and expertise into trying to find initiatives that will align people, align staff, and patients to do this kind of approach.
In other words, I'm very much interested in bringing people together, bringing the minds together, and working around own frameworks that will surface challenges in the healthcare system, and then we, together as a group, can find the better solutions. So we use specifically designed thinking around human-centric approach which is considered a different kind of research approach, a qualitative kind of research, where you really need to go dig deep inside into the services, and the systems, and the blueprint of the hospitals and the journey of the patients to try and understand where are the pain points of the system and the customers. Whether you define the customer as a patient, or staff, or a member of a family.
So currently we are all working to educate King Fahd Medical City staff and front liners specifically how to use design thinking as an approach to surface the challenges and then bring the best solutions out of that. This is just the beginning of the pipeline of innovation. Once you have the solution tested, and prototyped, and iterated, and in place, you then really need to test for patent, or intellectual property, and protect those rights for those inventors. And after that you need to commercialize this kind of product and hopefully get it licensed. And then you can go ahead and start as a startup and mature this kind of project to be scaled up outside the hospital.
So this is basically the main kind of research approach that I'm doing. It's more about human, it's more about gathering qualitative data from the system itself to try and define challenges for better solutions.
DR. SEBA NADEEF: That's great. What about you, Dr. Malak, since you are a physician and scientist at the same time?
DR. MALAK ALTHAGAFI: I think 2020 was one of the busiest years in my life as a physician, as a scientist, and even as an executive. I was trying to make it a little bit more simply, so I will just dissect it more. So as a physician, a pathologist, I've been involved in the selection implementation of different molecular diagnostic essays, and tools, and signing out some of some of these reports. So that's my role as a physician.
As a scientist, a researcher, I am the primary investigator with another wonderful lady in a project called--
[BACKGROUND CHATTER]
--in a project that looked at the health genetics of COVID-19 patients in Saudi Arabia. So from the international figures, we know Saudi Arabia ranked third in the lowest countries with fatalities of COVID-19, around 1% only that people who died from actually COVID-19 in Saudi Arabia. So we are studying different genetics variation and factors of what could be the cause of this. And we have very exciting results which will be in pre-print in the next few days on hopefully online and in journals after that immediately.
I've also been working as a Co-PI with different scientists here in the Kingdom. Its, KAUST, King Abdullah University of Science and Technology and others. And validating a new diagnostic tool, mainly the point of care one, using different genetic technologies like CRISPR for example, the paper was online a few days ago called Eye Scans, you can find what we do. We basically use CRISPR technology to come up with a faster, lab-free kind of approach, a very cheap approach. The other one is working with using peptides techniques to also come up with a very accurate, more sensitive and specific COVID-19 [INAUDIBLE] care testing.
So that's what I do as a researcher. Now as executive, that was the busiest part of my life this year. From the beginning of this, I've been working very closely with our president, Dr. Anas Al Faris and the VP, Dr. Abdulaziz in developing a comprehensive, strategic innovation program related to infectious disease action platform in Saudi Arabia. The heavy documents, some of it will come online in the Lancet Health soon and others have already gone to higher leadership for review on implementation hopefully.
The other one I've been also involved heavily in my prior position as a Deputy Director Scientific Support And Innovation. I worked heavily in developing a program that called for a fast track for COVID-19 research, implemented by KACST. We received over 500 applications, funded 50 or over 30 million Riyals. The idea here is to come up with the solutions for COVID-19 in different areas including diagnostic, AI, surveillance, epidemiology, [INAUDIBLE], et cetera within six months. The last other thing I did, we established a collaboration between KACST tax and Princess Nourah University to do accelerated testing within eight hours for all passengers going to King Khalid International Airport.
And also, a few days ago it was announced in the news finally, at least what related to COVID-19 and other work was all the work we've been doing with the S20 as part of G20, because Saudi Arabia's a host this year, and Dr. Anas is a chair of S20, so I've been working on task force one [INAUDIBLE] future of health, and also in the policy paper, as well as we would love to have all of you as attendees to the next week last webinar of Women in Science where I will be the moderator, and we will have extraordinary, distinguished women from all over the globe. So that's me in a nutshell, what I've been doing in this year.
DR. SEBA NADEEF: Actually, this is very impressive. I know 2020 might be hard, but it's still very impressive, I can tell you that. So what about you, Dr. Mariam?
DR. MARIAM ALEISSA: Well I don't think I have much as everyone else since I just arrived last April and we faced this pandemic. However, I would like to talk about my experience in translational medicine. I was working in research within MIT or during my PhD in finding a genetic variation associated with a certain phenotype.
And this kind of research takes a multidisciplinary action involving from taking the sample from the patient into the lab and then from the lab doing functional biology, bioinformatics, and pathway analysis. And from there back to the clinic where there's other stuff that will be involved and the patient himself. Like observing, trying to create a diagnostic tool, or medication for a certain problem.
DR. SEBA NADEEF: Thank you very much. And last but not least, Dr. Sana?
DR. SANA AL ATTAS: OK, since I'm an Associate Professor in Biology most of the efforts are being divided between teaching undergrad students and postgraduates learning programs. I'm working with my students and other colleagues in a number of research activities that involve multidisciplinary experts which in is a form of translational science. And applying, of course, the findings from these researchers to enhance the health and well-being in humans.
DR. SEBA NADEEF: Thank you very much. Actually it's very impressive and informative to see how can different backgrounds serve for the same need or the same scope in the translational research area in Saudi Arabia in terms of science, research, innovation, and techniques. But maybe we would like to know what is the current state of translational research in the kingdom? Maybe, Dr. Malak, you can help us with this question, because I think you're are more open in your field and your schools to different areas. So what is the real state of translational research?
DR. MALAK ALTHAGAFI: So we'll focus only on this and the healthcare for this session. So if you would imagine with me, as many of you know, when we talk about the innovation ecosystem, we think about three parts-- the R, the research which is mainly basically research done by the academic, usually the universities get a paper out of it or a patent. And then we have the development, which I have translated here as a translational research. Which is, for example, healthcare means we do clinical trials, and also we do, for example, prototypes for medical devices or, for example, a demonstration platform for diagnostic tool, et cetera.
And the last one is industry deployment or commercialization. So we'll focus on the middle one-- translational research or the development part of it. Where we are today in Saudi Arabia, I will give you a very honest answer. We've been doing great in the R part, we are doing well, we are ranked around, if I remember, 32 or 30 nature index. We're one of the best countries in getting papers in high impact journals, even in healthcare.
Now when it comes to development, people call this area the value of death, and this is true. Because this area is where we have limited funds from the private and public systems, and it's even worse in Saudi Arabia. For example, the number of clinical trials, as I just told you, it's one of the translational areas, we only that 400 clinical trials over the last 10 years in the kingdom. Compare it, for example, Singapore, 1,700. India, 2,800. I don't want to even say what the number is in the US, but can you guess? 80,000.
So we still have a lot to go with this kind of translational research. Publication, I told you, we did well. It's not large in quantity, but in quality, we did around 1,300 papers in 2017 related to healthcare, average citation around four, so this is good. Now talking about patents. What we did, so if you looked at this information, per how many patents you feel per 1,000 researchers, we did actually very poor over the last five years. Only 48 chemical patents which is not acceptable at all.
So here where we are today in this healthcare, and as I mentioned this is a global problem, it's not just a Saudi problem, where both government and private sector have to work together to build infrastructure, because this kind of infrastructure labs is different than academic labs. And also, build a human capacity in this area, and build more coordinated, integrated effort between the different stakeholders and put more regulations that help everyone to do well.
DR. SEBA NADEEF: So I think, from my opinion, there is a great effort from the kingdom to support research, but maybe that strategy should change or we need to do a lot to advance the translational of research. So it comes to my mind, what do we need to advance the translational research? Or what is the gap? Is it, for example, the communication between universities, and hospitals, and companies to work all together to reach a specific target? Or what do we need to do in order to develop the developments and manufacturing in the kingdom by attracting big pharmaceutical companies? Maybe Dr. Sufana can help us answering this question to think what can be done to improve or advance the translational research?
DR. SUFANA ALMASHHADI: I think it's a very critical question, and as Dr. Malak was saying, it's a global issue, it's not only a local one. But the formation, as Dr. Malak was saying, of an ecosystem that harnesses, and supports, and embraces this type of research that is very impactful, this is what we need. So we really need to have a better kind of communication, which comes in the form of regulations and rules of engagement between the academia and research between the policy generators and regulators [NON-ENGLISH SPEECH].
And then lastly, the commercial side or the industrial side of producing those products and maintaining them into the translation side or the bedside. I guess that Saudi Arabia is one of the countries that very much focuses on the input of things, the number of research projects, the number of patents, but we don't necessarily think about what is the real impact on the society? Because we don't start by addressing the gaps, and the challenges, and the needs. We think about solutions, and our assumptions, and what our kinds of conclusions, and then we work on them.
But the moment that we try to transform those patents into real life projects, we find that they are not being able to sustain commercialization, because they haven't addressed a job or they haven't addressed a need from the beginning. And that's why even in the Global Innovation Index of Saudi Arabia and the rest of the world, gladly this year Saudi has itqadamat o ithasanat advanced by four levels. Last year it dropped even more than six levels, just because it shows that we focus so much on our inputs and we focus a lot on the number of patents that we are producing, but we don't focus much on the impact and on the output.
So I guess by real communication and addressing-- specifically we are talking about translational research and healthcare-- if we start by working on the challenges and the obstacles first, and then we go back and form our projects in a way that addresses those challenges, I think we would see better impact and better sustainability.
DR. SEBA NADEEF: Yeah, I totally agree with you. But what, in terms of education, maybe Dr. Sana, from your academic point of view or experience, do you think creating new tracks like MD ad PhD programs where medical doctors are also involved in science and research it can be more critical, more beneficial. Or do you think we have already the human power, but we need just to change the strategy?
DR. SANA AL ATTAS: Yes, I think yes, indeed, why not. I found that top universities worldwide are doing the same thing. For example, the University of Edinburgh, University of Berkeley, University of San Francisco. In England we find the University of Liverpool, King's College London, Imperial College. They're all designing to cover major areas of modern translational science including drug development, genomics and development of the skills related to research and data analysis.
It also improves the ongoing knowledge and skills for clinicians and scientific professions at all levels. So I think it will be an idea in the right direction if it really happens here. That is my answer.
DR. SEBA NADEEF: Yes, I totally agree with you. And actually, talking about translational research, maybe it's more realistic if we give a clear example of what's happening. And I don't think there is a good example better than COVID-19, because it's science, it's research, and finally, the entire world is trying to develop a vaccine. So today we have COVID-19 pandemic, and many countries are working toward different strategies to develop a vaccine, improve the diagnosis of the virus, or even establish technologies that it that are needed for facing this pandemic. And now it's the time to move faster than ever, as they say.
So here where it comes the translation and research, and we know that in Saudi Arabia we contributed a lot to face this pandemic in terms of prevention and also supporting research. So maybe Dr. Mariam can tell us, from her experience, in terms of research, fund, and working in research. How did Saudi Arabia face this pandemic?
DR. MARIAM ALEISSA: Well, on the research aspect, the government funded generously research during the pandemic through different governmental institutions like the KACST, KAUST and the Ministry of Health, Ministry of Education. K Mark as well and the CDC have been involved as well. This is not only on a statistical, or let's say surveillance, level, it was beyond that, involving wet and dry labs by creating a number of innovative tools. Like if I could talk about the artificial intelligence where there is a number of ideas that have been proposed, and a number of things have been presented like applications-- like [Arabic], and [Arabic], and the Saudi dashboard as well was one of the things that have been produced during this pandemic.
And beyond that, going to the lab, a number of, let's say attempts to try to find a vaccine as well have been established in different institutions. Innovative ideas, like creating-- as Dr. Malak said-- a diagnostic tool which is cheap, available, used as a point of care have been established by KAUST Which is called, I think, [INAUDIBLE].
Also at a clinical level. anything produced worldwide has been also implemented. It's like trying to import any new therapeutic method or medication to solve the problem by using plasma as a treatment. Taking those plasma from most infected individuals and treat the ones those who are in critical condition. Also, a lot of research has been applied whether in the virus or the host, and I think Dr. Malak has talked about the human genome initiative.
And also, I think Dr. Sharif Halam mentioned something which is like collaboration. Yes, there is some collaboration between institutions. However, I think we need to do this in a higher level, and we need regulations as well since everyone, I think every institute wants to take the lead in something. However, this is not about institution, this is about national security and a pandemic. Yeah, that's it.
DR. SEBA NADEEF: What about you, Dr. Sana? I think from your experience you can tell us more about collaborations, whether with universities or the Ministry of Health to face the pandemic.
DR. SANA AL ATTAS: Yes, indeed. So since the beginning of the COVID-19 19 pandemic, the kingdom of Saudi Arabia has stood up to tasks of finding those that are infected with the virus and treating them. Efforts are yielding fruits in that the number of cases daily and the cities of Saudi Arabia has continuously declined. Light must be directed, honestly, to the government support for the Saudi University by giving opportunities to researchers with financial support to conduct research from several disciplines to confront this pandemic.
King Abdulaziz Centre for Science and Technology, which is KAUST the Ministry of Education, represented by I think 17 year universities if I'm not mistaken. Or I think it's between 17, up to 21. And the Ministry of Health as well have launched grand programs to support COVID-19 research. King Abdulaziz University was able to isolate the virus. I have to mention that also the Ministry of Health in Saudi Arabia continues its efforts to combat the COVID-19 pandemic as it has already originated efforts to develop an effective vaccine for the disease.
Moreover, the Ministry of Health also is conducting experiments and research in vaccine development. An announcement has been made that there would be a clinical trial for a vaccine against the virus which will be conducted in the kingdom within the framework of that cooperation agreement between the kingdom of Saudi Arabia and a Chinese company, I think it's [INAUDIBLE] and other collaborations as well which managed to develop a vaccine against the virus.
I think that the first and second basis of the vaccine trial has been done in China and other countries while the third phase will take place in the kingdom. Also the Ministry of Health has stressed that the launch of the study will be announced very soon, and this step is a continuation of the studies and research as the Minister of Health which often conducts in this field. So it has also recently cooperated with the WHO to conduct an advanced, multi-center clinical study in several hospitals in the kingdom to combat the spread of the novel coronavirus pandemic.
So honestly, the kingdom of Saudi Arabia is making a great deal of effort to keep the citizens and residents safe from the COVID-19 threat. Over to you, Seba. Thank you.
DR. SEBA NADEEF: Thank you, Dr. Sana. Actually it's very impressive to know all these contributions behind the screening and what the Ministry of Health and the others are doing in order to face this pandemic. Sometimes it's not said, but it's good to know what is the real state. But what about the technologies, Dr. Shada? What about employing innovative ideas or deploying new technologies? Do you think it can be approached [INAUDIBLE] the pandemic?
DR. SHADA ALSALAMAH: Absolutely. Well, thank you, Seba. Technology goes hand in hand with people, and human resources, and efforts coming from people, because it's supposed to help people manage things in a better way. Let me start off, before I answer this question, by giving a highlight showing the current state of the Saudi Arabian's digital health strategy where currently we're actually at right at the middle of a shift to fully digitize sectors. And healthcare is on top of that.
And having a fully digitized sector with the right infrastructure and resources is actually at the core of Saudi Arabian's vision 2030. This is mainly, I'm speaking from one of the perspectives, to connect the autonomous and distribute information silos in all sectors, but mainly in healthcare since it's a very distributed sector in order to allow making informed decisions. And that's specifically from a technology perspective.
Now although it has been extremely challenging to combat COVID-19 which needs collaboration and information coming from all of those systems, from 13 different regions in Saudi Arabia, without having such infrastructure ready, I think and I believe-- and I'm going to show that in the webinar by explaining-- how the kingdom has done a fantastic job in utilizing technology and emerging technology in many ways during the pandemic.
And I'm going to highlight two specific examples to show two different stakeholders, how the technology empowered healthcare decision makers. Whether there have been regulators, healthcare providers, or even payers at one end of the spectrum. And also another example to show how the patient at the receiving end of that spectrum has been empowered as well by the kingdom to manage and combat, to play the specific role.
Now, when it comes to decision makers, one of the two examples I want to demonstrate, they were under a lot of pressure trying to ensure that the total number of COVID-19 19 cases does not exceed the current healthcare capacity. And we're talking about hospitals across 13 different regions in Saudi Arabia. And then we're talking about over 33 million people. So they were equipped during the pandemic with really great tools in order to raise the healthcare capacity line in different hospitals based on available resources. And also to increase the capacity line and also flatten the coronavirus curve with the use of technology.
This is by monitoring, mainly, the three main factors contributing to managing it from a technology perspective-- the workforce, the infrastructure itself-- bed capacity and bed management-- and thirdly, the medical supplies. So these are the three factors where they managed to monitor available supply, and numbers, and availability, and even competency when it comes to the workforce across all hospitals in the 13 different regions in Saudi Arabia.
And with the help of technology, they managed to do that with a level of granularity that can be on a single patient case where they have to decide where to refer that patient from one hospital in one city to another one within the time-frame that would allow room for her safety. Two, the whole country level of management of the bed capacity and medical supply across the country.
This is to best manage the resources needed for 40% of COVID-19 cases according to the World Health Organization. Those are the 40% of COVID-19 patients that needed hospitalization depending also on their severity level. So that's how technology helped decision makers. When it comes to patients, it played a great role in implementing patient centricity through a number of mobile and personal health applications. The government actually implemented and made available during the pandemic, and enhanced some of the existing ones and built other new ones. And they were more mostly needed during the pandemic.
This is to mainly support patients diagnosed with COVID-19 and their kids or their caregivers throughout the treatment journey of those patients staying at home mostly which is you know the 60% of the patients who don't need hospitalization. And there is no better way than to explain and demonstrate that than telling it from a patient's personal experience.
My father, Dr. Abdullah Alsalamah, who I hope is joining us today, he developed his first COVID-19 symptom in June 20, and we all have been, as a family, been on a roller-coaster ride for over 60 days until he got discharged from the hospital on July 15 and self-quarantined for 14 days. Now I'm going to tell you the story from his perspective, like he said it. According to his journey, it went as follows.
It's divided into chapters-- the first chapter, first scene, over a live chat with a Minister of Health accredited physician using the e-health app which we name locally [NON-ENGLISH SPEECH], when he developed his systems and after a few Q&A exchanges between him and the physician, he was diagnosed with COVID-19 and also provided with a list of suggested or nominated nearby centers to have a confirmed test in order to confirm the positive case.
After that, once he was given that information and diagnosis over the phone, he informed the family and also self-quarantined, because he was a mild case at the very beginning. Until his symptoms got worse, this is when he called the national health hotline-- 9-3-7, because it was within working hours. So they answered the phone, the chat wasn't working at the time, but there are options available 24/7 for all citizens. And he spoke to another doctor-- or let's say an accredited physician-- who also confirmed the diagnosis, that was days later, prescribed medication to manage his symptom over the phone, and also offered to deliver during their curfew hours when no one was allowed outside their homes. And he also advised him to go to the nearest hospital if he did not feel better after taking the medication prescribed.
Which is exactly what he did. The very last chapter, and he got tested and went to the hospital and was admitted there. Now the funny part is that the last application or technology, mobile application he used which is called a Rest Assured, after being discharged from the hospital where he was referred for to home quarantine. So he was automatically registered in Rest Assured, or we call it [Arabic] application where they sent him a flood of messages. And he was complaining about the volume of messages that he received from the application once he left home and went for a follow up at the hospital. This is where he needed to change his location in the application, because they were monitoring the self-quarantine at home.
And this was a wonderful example showing you know how different tools were used. And he did not have to actually go and see someone about those, those were done from home and he didn't have to leave home unless for hospitalization. And also throughout his journey, us, the caregivers, generally the citizens and also the patient himself, were given really good advice and valuable hints and advice from the ministry to give to help him best manage the case and avoid the spread of COVID-19.
This is one simple example from personal experience to demonstrate how the kingdom has orchestrated a great technology enhanced suite to empower personal health for over 33 million people and reduce the burden on their caregivers and also the health system. Thank you very much, and over to you, Seba.
DR. SEBA NADEEF: Thank you very much. Actually it's very magnificent to see how technology served to face this pandemic behind the stage, as they say. But sometimes people do not look at the effort, sometimes people only look at the outcome. Like why we did not reach this stage? Why we did we not do that? So this take us to the next question that everyone is asking-- what is the vaccine? Or why does it take so much time to develop a vaccine? Although we, in the kingdom, work on it in a different way-- not necessarily developing a vaccine, but characterizing the virus or collaborating with people from the outside.
But taking COVID-19 of an example, it's taking almost a year to develop a vaccine, and we are not sure yet of the outcome of this vaccine in terms of side effects and how friendly it is. And some of these vaccines are taking five to 10 years. So my question is, what are the challenges behind the timeline of producing or developing a drug or vaccine generally? Not necessarily only in the kingdom. Maybe Dr. Sufana, you can help us answer this question?
DR. SUFANA ALMASHHADI: Yes, so obviously we're trying to find a vaccine for a human disease. So it's a disease that is affecting humans, and whenever you are dealing with humans, it's always very complicated. And it's basically a safety issue that it's taking such a long time. Research is gradually accumulating very crucial data for us to understand the nature of this and all its aspects and how it's triggering our systems. So obviously we can see that COVID-19 is evolving, it's changing.
We didn't understand yet why it isn't affecting children as much as it's badly affecting adults. And we've heard about people and research saying that the virus that affects the Middle East, for instance, is different from the one that's affected Europe, different from the one present in the Far East. So research is still in its very initial steps and trying to accumulate data and understand the nature of this virus. That's why it's going to take a long time to find the vaccine and test it first. And several clinical trials are ongoing as we speak, but I think it's the safety issue that is why it's taking a long time.
DR. SEBA NADEEF: Yeah, I totally agree. And do you think, Dr. Malak, based on all this research, and technologies, and association that we are building to face this pandemic, can we use the same approach to use it for facing common diseases in our country? Like chronic diseases or infectious diseases in the kingdom? Or is it always different and variable?
DR. MALAK ALTHAGAFI: It's a very tricky question if you allow me to do. And people ask you, where is the vaccine? This is actually, and I think many of the audience would agree, it's the first time I think in a century the whole world is working on one health problem. We have not seen this since the Spanish influenza or any other major things which hits the entire world. And with this, it takes time. And as Dr. Safana said, safety comes first here. You're not designing a therapy for individuals. So this is not a therapy to cure a disease, you're giving a vaccine to the entire population. So any small side effects would have a major impact.
Now, going back to your to your question, the process of developing drugs is not a short process, as you said-- five to 10 years, sometimes 15 years. And the history tells us and also the current, did we find a cure for all cancers? And we know cancer for many, many, many years, and even with some reported before, BC kinds of cases that got reported. Did we cure it? No. All the cancer? No. Did you cure diabetes? No. Did we cure any of these other common things? Not only Saudi, world-wide. No. It's a very complicated process. Many factors are involved-- individual genetics, epigenetics, environment, lifestyle. It's a very complicated thing to come up with a treatment or treatment for these complex diseases as we call it.
Now, I will give you an example. The lifecycle of any-- if you want to create a drug, for example. You need basic research. This can take many years and somebody needs to know what's going on, and then you need a drug discovery phase where you're lucky, you have a target now. Now let's test this target, let's lead, and try to understand more, and do preclinical study on animals. No human testing at this stage. This, again, can take years.
Now, you're lucky, you pass preclinical and you go into product development. You want to go to the human testing-- phase one, clinical human, small group, 2,200. See if it's safe, and the dose, what is the dosage required? If you're lucky, you move to the second phase. Proof of concept, more people, around maybe 300, maybe take one or two years, drugs who reach this phase, 33% of them, will proceed to the next phase, so you've lost already two thirds.
Phase two and three, again, now you're looking at 1,000 new people, looking at what side effects can come to you, and usually it takes to four years, and not many drugs pass this stage. And even if you're lucky and move to the market approval, it takes some time, and many drugs we know have been withdrawn from the market. So this is what we are talking about. This is the journey of any drug or vaccine. It's not an easy one.
So I'm going to switch examples to something that maybe we thought, as a geneticist at least-- and we're very naive on this-- when the Human Genome Project completed after 13 years in 2003, we thought we thought we would solve all the genetic issues. We were wrong. Now it's 20 years after almost, and there are very few diseases that we could find some sort of cure for.
So now in Saudi what we did, we realized now OK, there is enough research being done maybe in discovery, now let's do the technology development part. And that's what we did with the Saudi Human Genome, it was a technology development part where we brought the technology, trained it, discovered what's common in our population, and now we're moving to the third phase which is commercialization, hopefully, by having a product to prevent these diseases, because we know it's still a long journey to cure them. So let's prevent them by expanding our pre [INAUDIBLE] screening for genetic disorders by expanding our newborn screening, by having more advanced diagnostic tools to detect these diseases during and even before marriages or even very early on when a child is born.
So this where we are standing. And this is why we thought it's not complicated, because usually genetic disorders are monogenic and caused by one mutation.
DR. SEBA NADEEF: Yeah, I understand the pain behind it, because I'm a researcher, but I wish I could make all this dialogue in a simple word and publish it to the public and tell them, look, this is the effort behind that and still it's not very clear. It's always critical and very challenging, I totally agree. But what about the economics, Dr. Mariam? We know that the COVID-19 pandemic had far reaching consequences beyond just the spread of the disease itself. One of the aspects is the economic impact. So how can we take a steadfast decision during the crisis to employ innovation, ideas, or new technology to advance the healthcare?
DR. MARIAM ALEISSA: We did a great job actually in Saudi Arabia. economic were affected around the world, and everyone was trying to find the solution for this dilemma. Nobody knows what to do and which is the best approach to reach. However, in Saudi Arabia we took prompt action to create policies and regulations not only on a health level, also on governmental level. At the same time, moving the economy wheel and finding solutions to make things active by finding, as an example, making people work from home, and regulating work hours, allowing those who need to be on the field for a certain time, and others to stay at home.
Also, to reduce the economic burden, the Ministry of Health prioritized hospitalization for those who really needed to be hospitalized while the others can be quarantined at home. The testing, as well, has been reduced in a great amount by using the applications where Dr. Shada mentioned that you can evaluate yourself and know that you need to be tested or not. And also finding cost-effective, new technology and innovative ideas in the economy.
Yes, we did a lot. However, I think learning from this experience is really valuable. We need to take notes and learn from the things that happened during this pandemic. And I think one of the funniest things that's happened during the pandemic is the mask and sanitizer crisis where people were trying to save as much as they can at home. And this also was a privilege for some of the merchants to not sell in irregular prices and try to increase the price.
The government played a good role in that, actually a great role, and it was a bonus for us by controlling the prices and supporting manufactural companies to at least cover the kingdom needs from sanitizers and masks. So we were self independent on that. Hopefully we were doing in different aspects, and technology, and other stuff. It's like keeping an eye on the world and observing, learning, and at the same time, the other eye watching, and monitoring the situation within Saudi Arabia. Yes, we did a lot, but we need to learn and find a strategy for anything in the future. God forbid, but we need to learn.
DR. SEBA NADEEF: Yeah, that's really great. And we all agree that this pandemic is surprising, and it was unexpected for the entire world. So maybe, Dr. Sufana, you can tell us if you think this crisis opened the door for us to think in advance how to face the risk of any future pandemics or any waves that could possibly hit us, which is I hope not in the near future.
DR. SUFANA ALMASHHADI: As Dr. Mariam was saying, there are lots of lessons learned throughout this experience on a personal level, team level, organization level, and even national level. Yes, it's very hard to predict what's going to happen in the future, especially that specifically dealing with COVID-19, it's something that has never happened recently, and we don't have reference, data, or memories to refer out experiences or, how did we navigate so this challenging time? I'm speaking on the level of organization.
So the last pandemic, as Dr. Malak was saying, probably was the Spanish flu, and it was more than 70 years ago, so we weren't even there. So we don't have that kind of experience and the know how to navigate this. Over from an innovation point of view, I believe that there are some theories that you could work with to predict what's going to happen in the future. And it's just not in the terms of health crisis or pandemic, but it's to let you know what are the gaps and to anticipate, well, what do you need so you can shape your business towards that? At least you can try and sustain your business in this challenging, highly competitive time.
So I can speak briefly about one of the theories that I think, specifically in healthcare, could be very helpful is that the Theory Of Disruption found by Professor Clayton Christensen. So specifically in healthcare, Professor Clayton defines the Theory of Disruption is that you make the complicated simple and the expensive affordable, which means that you make the complex healthcare services that are only being provided at the large healthcare complex systems, make them simpler and more accessible, so you can include larger groups of people. People who cannot come to the hospital to get this access of care, they would have access from the comfort of their homes or even from the rural parts of the country.
We can see this acceleration of application that happened during COVID-19, specifically in activating virtual connections and virtual clinics. So this is specifically and mainly the Theory of Disruption where you have allowed people to get access to care not only by coming physically to the headquarter or the healthcare care hospitals. So if we have anticipated that we need this kind of access of care for people from their comfort of their homes long time before, and we have activated the systems in a way, we could have navigated this challenge maybe smoother, maybe at least reassuring patients that they are not disconnected from their healthcare providers.
I'm not saying that the kingdom haven't done a great job. Yes, it has done an amazing job in adapting and shaping themselves in a quick way to activate this kind of care. But I see that this is a must. Don't rely on your business as usual, as it's going. Try to learn from this challenge, and try to mindfully and selectively shape your creativity and innovation in a way that it will serve challenges as we go through.
DR. SEBA NADEEF: Yeah, I totally agree. Before we close, do you think, Dr. Sana, would you like to add anything regarding what lessons have been learned from the COVID-19 pandemic?
DR. SANA AL ATTAS: Yes, thank you, Seba. Can you hear me? Can you hear me?
DR. SEBA NADEEF: Yes.
DR. SANA AL ATTAS: OK, so I think that this emerging pandemic shows that humans are not infallible, and communities need to be prepared. So like any other nation, worldwide, Saudi Arabia has learnt a lot. From basic universal precautions like hygienic ways of living, and handling infections, such as the common cold and flu, have tremendously improved that at individual, families, and household levels.
The transdisciplinary one health approach involving professionals from many disciplines such as medicine, veterinary, environmental health, and social sciences has been suggested as a means to limit new infectious outbreaks. Actually, the global experience is teaching that containment measures and the aggressive contact tracing is mandatory to keep the infection under control until an approved treatment or a vaccine is available to the global community.
Meanwhile, we learned the lessons of protecting the most vulnerable individuals and to rally around the signs. And I think that this pandemic has demonstrated the importance of research activities. Back toy you, Seba.
DR. SEBA NADEEF: Thank you very much. We've reached the end of our webinar, and before we close and we reach out to our audience and their questions, I would like to thank Dr. Kamal for joining us today and our distinguished speakers for enlightening the seminar. We appreciate having all of you here to cover this mysterious and interesting area and make it more clear for the audience. And also for us as researchers from different perspectives, because it was very informative where we think we are sometimes working alone.
So we need, from time to time, to know what the others are doing and to contribute as a group and not only as one person. So thank you very much for your time. Now I will go to the questions, and some are already answered, so some are still--
THERESA: I think there's a lot that are already answered, but could be answered in more depth.
DR. SEBA NADEEF: Yeah, so I'll start from the end. One question for Dr. Malak, why the Saudi Human Genome Project is not for the public yet? And the second question, are there any governmental rules or restrictions for publishing human sequencing data to the public?
DR. MALAK ALTHAGAFI: Thank you. I'm not sure why it's not for the public. Actually, the project was created for the public and for all Saudis That's the whole goal of it, to be for all Saudis. We have now reached over 60,000 samples, all of it collected from Saudi patients or volunteers. We have over 400 researchers who worked on this project from 72 institutions. So it is open. There is a dedicated website for it, and any researcher can submit that proposal, and it will be reviewed by a scientific committee to proceed with it or not.
But it's public, and there is actually another seven satellite locations in different areas in the kingdom. And King Fahd Medical City, where I oversee this one, in National Guard, and King Faisal Specialist Taibah University, King Faisal in Jeddah, and King Fahd Specialist Hospital in Dammam, and more recently, Tabuk University.
So the second part is, there is a restriction from the government about genetics data, and I'm not an expert on this, but the national bioethics committee takes this issue very seriously. That doesn't mean we don't publish. Many researchers publish what they find, but they make sure to de-identify and to keep the privacy of our patients. So we submit in the international respiraroty in the databases, and we do it. But it's not an open database for everyone, it's the Saudi Human Genome. It's only the PI can publish his work, making sure to stick to all of the ethical rules.
DR. SEBA NADEEF: That's great. Since the mic is yours, we have one question from Dr. Sharif of talking about collaboration. [INAUDIBLE] improve the collaboration, and there is a service through cracks to get away or advance the collaboration that we have, because, as you mentioned, we are facing a lot of problems that delayed the progress in terms of massive paperwork, a lack of fast delivery, low funds, and a lot of problems when it comes to the work that we have at the moment.
DR. SHADA ALSALAMAH: Yeah, thank you for this question, and I fully agree. And this is one of the exercises we did this year during the pandemic. We are trying to understand all the gaps we have in the system, and this was an obvious one. We actually don't have a central body or agency doing the national research development innovation coordination at a national scale. So due to this, we have a lot of duplication of resources. And even under-utilization of others and a lot of waste of time for many, many people-- researchers and even international companies.
So this is what KACST decided to take a lead on. We're not sure if this will be the only central national coordination administration or not, but this is what was established just last month. And I was lucky to be selected to be the director general of this new general directorate for National Research Development Innovation Coordination where we're trying to address all gaps, and more than this, trying to work with the regulators, with the university, with the research institute, with the international partners and national partners, and trying to make it a relatively easy journey for all researchers at different levels and different parts in the ecosystem.
DR. SEBA NADEEF: We have one question. Can you give a insight on the future of RNA based gene therapy in Saudi Arabia? It's an open question, would anyone like to answer? Maybe I can answer this question. Actually, I can say yes, because this was already approved like in the US and Europe, but there are a lot of challenges when it comes to when it comes to clinical trials. The same goes for the CRISPR testing.
A lot of improvement, a lot of challenges researchers are facing. Although the technique is there, we know how to design it, we know how to do it in the lab, but when it comes to the advanced stage when you want to apply it for certain diseases or you want to apply it for clinical trials or in a patient, still we are struggling with a lot of problems.
So as a technique, yes. But we do not know what are the challenges yet. And we hope it can be the [INAUDIBLE] and can be used as a therapy in Saudi Arabia. Do we have other questions? Yeah, actually we have one general question that after talking about COVID-19, one is asking, do you believe we are going to have a second wave of COVID-19? And if we are, are we well-occupied to handle it? I'm not sure about the second wave, I hope not.
[CHUCKLING]
DR. MALAK ALTHAGAFI: Yes. I think the world is already is starting to face a second wave. We've been seeing data from Europe-- France, Spain, and the UK-- there is already another surge in these countries. I don't want to lie about it, I think it's coming, but I think the good news is that we are better prepared this time. The first wave is a hit, and the entire world were not ready for it at all.
I think now we're more careful, and also, we'll continue to follow these precautions. Wearing a mask, it doesn't cost anybody anything. But it has a huge impact. One paper published two days ago in New England, which I loved the idea actually, it said, this is our way to get crude vaccinated. Breathing in a small maybe particle of the vaccine through the mask will build immunity over time. And I love this idea, it came from UCSF, one of the authors. Maybe that's the true way to go until the real vaccine comes. But just wearing the mask and keeping the distance, it will keep us safer inshallah all of us and our families.
DR. SHADA ALSALAMAH: Yes, if I may comment on the question, provide an answer and comment and second you, Dr. Malak. We've seen the measures, specifically in Saudi Arabia, where they're actually locking all ports where travel is banned, and I think this is mainly a precaution to prevent a second wave. So whether the answer is yes or no, I think they're doing the greatest effort to try to prevent that from happening. And at the end of the day, the government can put some technologies available and a lot of efforts, and granting, funding projects, and researchers to work on related topics that can specifically target COVID-9 from an individual perspective maybe the disease itself or it could be to help support the management and combat the disease.
But at the end of the day, all of us play a great role, like Dr. Malak mentioned, that can help us contribute to this overall effort. We cannot have a successful story to tell at the end of the day if we don't all participate and collaborate collectively to achieve that.
DR. SEBA NADEEF: Yes, thank you very much, ladies. I think we are out of questions, and we still have a few minutes before the end of the webinar. So I would like to thank all of you and would like to hear from you if there is anything that you would like to add-- insights, anything that you would like to add that we did not maybe cover during the webinar, please feel free, the mic is yours.
DR. SUFANA ALMASHHADI: Maybe I would add something about the previous questions about we are prepared to face another wave of COVID-19. I would say on a strategic level, King Fahd Medical City is just about to launch its new strategy for the next coming five years. And the strategy team have added a main program as a disaster management, and they have given it a lot of weight, and we will dedicate a lot of resources to handle that.
So I guess we cannot prevent another wave or a different type of disease that's going to happen. This is the new out of world wars that is coming, as Bill Gates predicted. So I guess the only solution is that we have ourselves and our organizations well prepared, especially the healthcare sector.
And I think this is really a great time for all of us to try and align our innovative efforts, coming together as a whole to try and test what could be potentially the solutions to navigate such a hard time.
DR. SEBA NADEEF: Thank you very much, Dr. Sufana, for your insight. Dr. Kamal, would you like to add anything before we close the session for tonight?
KAMAL YOUCEF-TOUMI: No. I just would like to thank you for moderating this webinar, and also thank all of the panelists for their contributions and clear explanations of the translational research as it relates also to COVID-19. And also to thank all the participants who are with us today, and I hope that we can see all of you in our next webinar soon. Thank you.
DR. SEBA NADEEF: [ARABIC]
From my side, I would like to playing all the attendees for their participation, and the people active in their questions. Thank you to the panelists for your time and your effort to be here and highlight the major achievements in the kingdom and globally and what is the state for Saudi Arabia in particular to face the pandemic.
I would like to thank you all for being scientists, for being ladies, for being brave, and to contribute or to support science and women in power in Saudi Arabia. Thank you also to the organizers, we cannot forget Dorothy, Nadia, and Theresa behind the screening for organizing this and the effort. And Dr. Kamal, of course.
I wish a lovely evening for all of you, and thank you very much, and I hope to see you all in our next coming webinars. There are people who ask about Arabic and how can they join. There will be webinars organized for such a purpose, and you can search it online. Ibn Khaldun fellowship to see what are the requirements to apply for 2021, it will be open October 1. Thank you very much, and good evening, everyone.
ALL: Thank you.